Understanding Peripheral Artery Disease (PAD)
In the realm of medical conditions that frequently elude detection until they advance to critical stages, understanding Peripheral Artery Disease (PAD) becomes paramount. PAD, a condition impacting blood vessels outside the heart and brain, often operates stealthily, progressing quietly. This article aims to shed light on the complexities of PAD, encompassing its prevalence, risk factors, symptoms, and the pressing imperative of early detection and awareness, all contributing to a better understanding of Peripheral Artery Disease.
Understanding Peripheral Artery Disease (PAD)
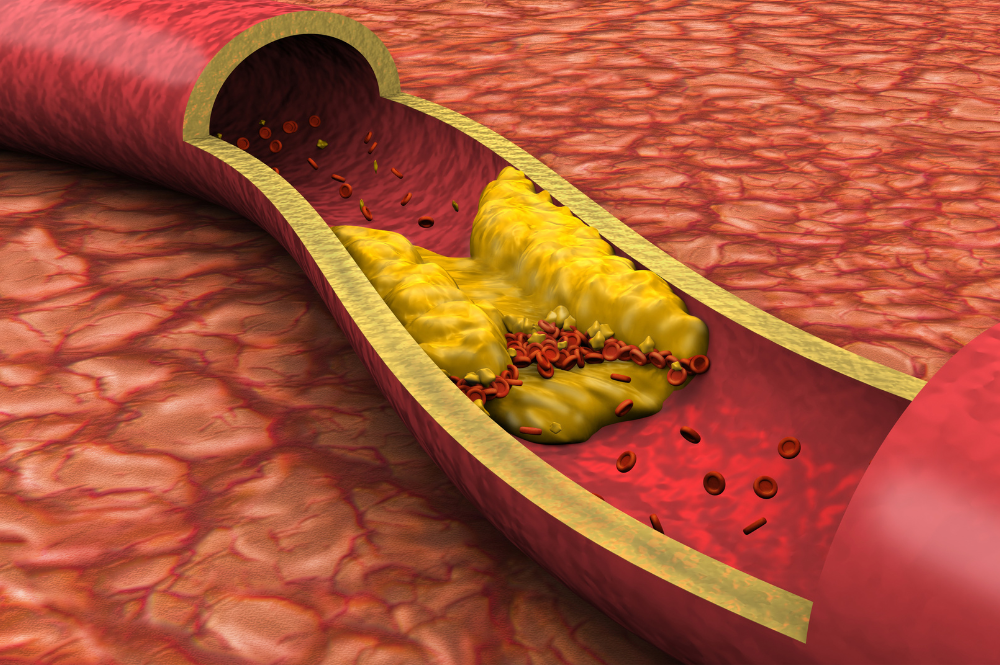
Peripheral Artery Disease refers to a condition where the arteries responsible for carrying oxygen-rich blood to the extremities—specifically, the legs and arms—become narrow or clogged due to the buildup of fatty deposits, known as plaque. This narrowing process, medically termed atherosclerosis, hampers blood flow, resulting in reduced circulation and various discomforts, including pain.
Often labeled the ‘silent killer,’ PAD has a knack for staying concealed. Unlike conditions with overt symptoms, PAD can progress stealthily, causing damage before becoming noticeable. Its silence lies in the fact that it doesn’t always present clear signs, allowing it to quietly advance until more severe issues arise.
The Prevalence and Hidden Nature of PAD
Despite its quiet presence, PAD is surprisingly common. Peripheral Artery Disease is present in over 12 million people¹ in the United States alone, and this number is expected to increase as the population ages and risk factors such as obesity and diabetes continue to rise. What’s even more surprising is that a significant number of PAD cases remain undetected. This happens due to various factors, including the slow progression of symptoms, lack of awareness, and misinterpretation of discomfort.
Unseen Consequences of Undetected PAD
When PAD goes unnoticed, it doesn’t remain idle. Instead, it evolves into a ticking time bomb, potentially leading to heart attacks, strokes, or even amputation. With inadequate blood supply, tissues in the extremities struggle to heal, resulting in delayed wound healing and, in severe cases, gangrene. The most dire consequence is amputation, highlighting the importance of early detection and intervention. Additionally, the insidious effects of undetected PAD can extend beyond the limbs, increasing the risk of heart attacks and strokes, emphasizing the urgency of uncovering this hidden threat.
Risk Factors: Who’s Vulnerable?
Certain individuals face a higher risk of developing PAD due to a combination of factors:
- Smoking: Cigarette smoking is a major risk factor for PAD, as the harmful chemicals in tobacco contribute to artery narrowing and hardening, accelerating the disease’s progression.
- Diabetes: People with diabetes are significantly more susceptible to PAD. Elevated blood sugar levels can damage blood vessels, leading to atherosclerosis and arterial blockages.
- Hypertension: High blood pressure is a common risk factor for various cardiovascular conditions, including PAD. Increased pressure on arterial walls can contribute to plaque development, restricting blood flow.
- High Cholesterol: Elevated levels of LDL (low-density lipoprotein) cholesterol and triglycerides can lead to plaque accumulation in arteries, reducing blood flow and increasing PAD risk.
- Age and Family History: Advancing age is a non-modifiable risk factor for PAD, with individuals over 50 being more vulnerable. Additionally, those with a family history of PAD or other vascular diseases have a higher likelihood of developing the condition.
Deciphering the Clues: Recognizing PAD Symptoms
While PAD’s silent nature poses challenges, it does exhibit telltale signs that individuals and healthcare providers should take seriously. Intermittent claudication, which refers to pain, cramping, or fatigue in the legs while walking, is a classic symptom. As the condition worsens, pain may occur even at rest, accompanied by other signs such as cool or pale skin and slow-healing sores.
The Crucial Role of Early Detection
The adage “prevention is better than cure” holds true for PAD. Early detection is key to halting its progression and minimizing its impact. Identifying PAD in its early stages enables healthcare providers to implement lifestyle changes, prescribe medications, and initiate interventions that can significantly improve blood flow and quality of life.
Barriers to Testing and the Counterargument
Despite its prevalence and potential severity, PAD testing often remains elusive in clinical practice. Several factors contribute to this challenge, including a lack of awareness among both patients and physicians, time constraints in busy medical practices, and an underestimation of the importance of gaining a comprehensive understanding of Peripheral Artery Disease. However, these barriers must be addressed. The counterargument, driven by the potential to save lives and prevent amputations, emphasizes the urgency of tackling this issue head-on.
Simple Testing, Profound Impact
The idea of testing for PAD might seem intimidating, but it’s surprisingly straightforward. PAD assessment, akin to taking a blood pressure reading, involves using a Doppler device to measure blood flow in the extremities. This non-invasive technique provides critical insights into the presence and severity of the disease.
Newman Medical’s Innovative Solution
One remarkable advancement in the field of PAD detection is the introduction of user-friendly tools like Newman Medical’s simpleABI. This innovative technology empowers healthcare providers to perform efficient PAD assessments with ease, contributing to the broader goal of early detection and prevention.
The simplicity and accessibility of the simpleABI are key assets. This versatile system streamlines the process of measuring blood flow in the extremities, making it accessible to a wider range of healthcare professionals. It doesn’t require specialized training, ensuring that more providers can participate in early detection efforts.
By incorporating the simpleABI into their practices, healthcare providers can play a crucial role in identifying PAD at its early stages. This aligns perfectly with our mission to raise awareness about the importance of early detection, which can lead to better outcomes for individuals and communities alike.
For those interested in exploring how the simpleABI can contribute to PAD awareness and prevention, you can learn more about it here: simpleABI Systems
Conclusion: Peripheral Artery Disease remains a significant concern, often lurking undetected until it reaches critical stages. This article has shed light on the intricacies of PAD, emphasizing the urgent need for awareness and early detection. Tools like Newman Medical’s simpleABI offer a user-friendly approach to testing, empowering healthcare providers to be proactive in the fight against PAD and its potentially severe consequences. Let’s continue to advocate for PAD awareness and take steps to address this hidden threat within our communities.
¹https://www.ahajournals.org/doi/10.1161/CIR.0000000000001153
