Peripheral Artery Disease Guidelines: 3 Key Aspects
Peripheral Artery Disease (PAD) is a common yet underdiagnosed condition that affects millions worldwide, particularly those over the age of 50 or with a history of smoking, diabetes, or cardiovascular disease. With that being said, individual should take time to understand peripheral artery disease guidelines.
For primary care providers (PCPs) early detection and appropriate management of PAD are critical in preventing serious complications like limb ischemia, heart attack, or stroke. This article will review the latest peripheral artery disease guidelines diagnosing and managing PAD, emphasizing the importance of using Ankle-Brachial Index (ABI) systems, such as those developed by Newman Medical, to streamline diagnosis and treatment in primary care settings.
Understanding Peripheral Artery Disease Guidelines
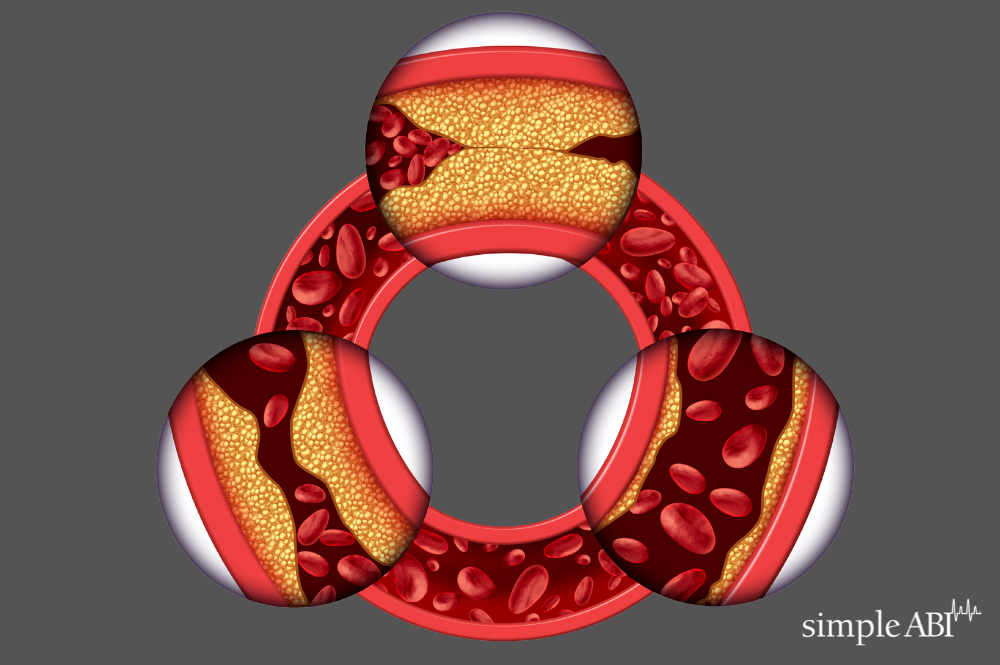
Peripheral Artery Disease occurs when plaque builds up in the arteries, leading to reduced blood flow to the limbs. This can cause symptoms like leg pain during walking (claudication), numbness, and in severe cases, non-healing wounds or gangrene. PAD is a significant indicator of systemic atherosclerosis, which means patients with PAD are at a higher risk of cardiovascular events.
According to the latest data from the American Heart Association (AHA) and the American College of Cardiology (ACC), nearly 8.5 million people in the U.S. suffer from PAD, making it a critical focus area for providers.
Key Peripheral Artery Disease Guidelines
1. Patient Assessment and Risk Factor Evaluation
The first step in diagnosing PAD, as part of the peripheral artery disease guidelines dynamic, is to assess the patient’s risk factors. The guidelines emphasize focusing on patients over 50 who have a history of smoking, diabetes, hypertension, or hyperlipidemia. Additionally, anyone with a family history of cardiovascular disease or those experiencing symptoms like leg pain during exercise should be evaluated for PAD.
Risk factors to consider:
-
- Age (especially over 50)
- History of smoking
- Diabetes
- Hypertension
- Hyperlipidemia
- Family history of cardiovascular disease
PCPs are encouraged to ask targeted questions about leg discomfort, non-healing wounds, or changes in skin color and temperature in the limbs.
2. Physical Examination
A thorough physical exam should be conducted to identify any signs of PAD. The latest guidelines recommend examining the lower extremities for:
-
- Weak or absent pulses
- Bruits over the arteries
- Poor wound healing
- Shiny skin or hair loss on the legs
- Coolness in the lower extremities
3. Ankle-Brachial Index (ABI) Testing
The ABI test remains the gold standard for PAD diagnosis in primary care settings. The latest guidelines reaffirm the importance of ABI testing, noting that it is a simple, non-invasive procedure that can accurately measure the blood pressure difference between the ankle and the arm. An ABI ratio of less than 0.90 is indicative of PAD.
The guidelines highlight the importance of using advanced ABI systems, like those from Newman Medical, which offer quick and precise measurements, allowing providers to diagnose PAD efficiently. ABI systems can also be integrated into routine check-ups for high-risk patients, ensuring early detection and prompt management.
Management Guidelines for PAD: Peripheral Artery Disease Guidelines
Once PAD is diagnosed, effective management is essential to prevent progression and complications. The latest guidelines recommend a comprehensive approach that includes lifestyle modifications, pharmacotherapy, and in severe cases, surgical intervention.
1. Lifestyle Modifications
Patients diagnosed with PAD should be advised on the following lifestyle changes to improve their prognosis:
-
- Smoking cessation: This is the most critical step, as smoking is a major risk factor for PAD progression.
- Exercise therapy: Supervised exercise programs, particularly walking, have been shown to significantly improve symptoms and increase walking distance in patients with claudication.
- Dietary changes: Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can help manage PAD and reduce cardiovascular risk.
2. Pharmacotherapy
The guidelines recommend several pharmacological treatments to manage PAD and reduce the risk of cardiovascular events:
-
- Antiplatelet therapy: Aspirin or clopidogrel is recommended to reduce the risk of heart attack or stroke.
- Statins: Cholesterol-lowering medications are advised for all PAD patients, even if their cholesterol levels are not elevated, to stabilize plaque and prevent further artery narrowing.
- Antihypertensive therapy: Blood pressure control is crucial in PAD management, with ACE inhibitors or ARBs being commonly prescribed.
3. Advanced Therapies for Severe PAD
For patients with severe PAD who do not respond to conservative treatments, the guidelines recommend advanced therapies, including:
-
- Endovascular procedures: Minimally invasive options like angioplasty and stent placement can help restore blood flow to affected limbs.
- Surgical intervention: In cases of critical limb ischemia, surgical bypass may be necessary to prevent limb loss.
- Wound care: Specialized care for non-healing wounds is essential to prevent infections and amputations.
The Role of ABI Systems in PAD Management
The use of ABI systems in primary care settings is integral to adhering to the latest PAD guidelines. ABI testing is a cost-effective, reliable method for diagnosing PAD early and initiating appropriate treatment. Newman Medical’s simpleABI systems, in particular, are designed to simplify this process, offering accurate results in minutes. These systems are user-friendly, making them suitable for use in both small practices and larger clinics.
The convenience of ABI testing in primary care settings ensures that high-risk patients can be screened during routine visits, allowing for earlier intervention. By incorporating ABI systems into standard practice, PCPs can significantly impact the outcomes for patients with PAD, reducing the likelihood of severe complications. This is where peripheral artery disease guidelines come in.
Conclusion: Peripheral Artery Disease Guidelines
Peripheral Artery Disease is a widespread condition with serious consequences if left untreated. For providers, staying updated with the latest guidelines on PAD diagnosis and management is essential. Utilizing ABI systems, such as those from Newman Medical, can streamline the diagnostic process, enabling earlier detection and more effective management of PAD.
Newman Medical’s advanced simpleABI systems are designed to provide fast, accurate results, making them an invaluable tool for primary care providers looking to enhance their PAD management capabilities. With early detection and comprehensive treatment plans, providers can significantly reduce the burden of PAD and improve patient outcomes.
This article reviews the latest Peripheral Artery Disease guidelines, emphasizing early diagnosis and management using ABI systems like Newman Medical’s advanced solutions in primary care settings.
Stay ahead of PAD management with Newman Medical’s advanced ABI systems—contact us today. Real people, real support, and solutions, from phone to field.
