The ABI-Q Advantage for Diabetic Care: A More Precise Approach to PAD Detection
Traditional Doppler ABI struggles with calcified arteries common in diabetics, leading to missed PAD diagnoses. ABI-Q with exercise offers a more precise approach:
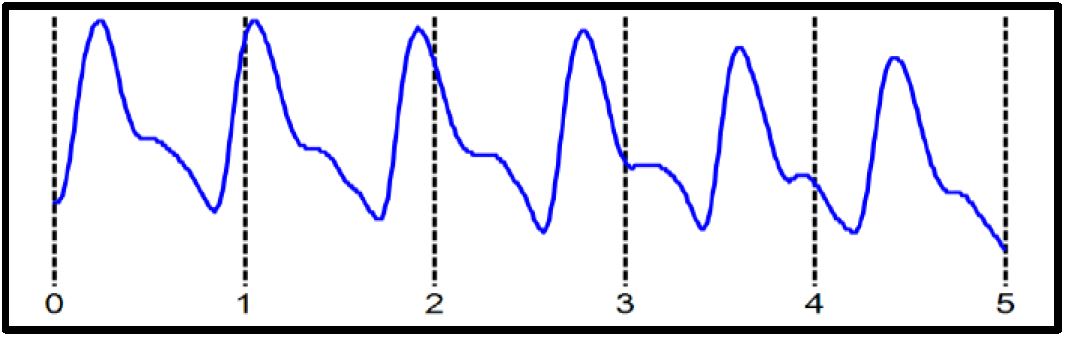
- Overcomes Calcification: Unlike traditional Doppler-based ABI exams, ABI-Q uses PVR waveforms unaffected by calcification, providing a clearer picture of blood flow.
- Earlier Intervention: Accurate PAD detection allows for earlier treatment, reducing amputation risk, heart attack/stroke risk, and mobility limitations.
- User-Friendly, Quick Exams: The simpler ABI-Q exam is easy to learn and fast, streamlining workflow and improving patient throughput.
- Enhanced Accuracy with Minimal Effort: A simple ankle flexion exercise significantly improves test accuracy while requiring minimal patient exertion.
Conclusions:
By addressing the limitations of traditional ABI testing on diabetics, ABI-Q offers a more accurate, objective, and patient-friendly approach to PAD detection. This empowers physicians with a faster, easier-to-use test that delivers reliable results. ABI-Q’s ability to overcome calcification, a common challenge in diabetic patients, allows for earlier intervention and improved patient outcomes. This translates to a significant reduction in amputation risk, heart attack/stroke risk, and mobility limitations for diabetic patients.
Newman Medical: Committed to Advancing Diabetic Care:
Newman Medical is dedicated to developing innovative solutions that improve the lives of diabetic patients, especially reducing amputations. ABI-Q with exercise exemplifies this commitment by providing a more accurate and accessible method for early detection of PAD, ultimately contributing to improved patient outcomes.
1.Creager MA, Matsushita K, Arya S, Beckman JA, Duval S, Goodney PP, Gutierrez JAT, Kaufman JA, Joynt Maddox KE, Pollak AW, Pradhan AD, Whitsel LP; on behalf of the American Heart Association Advocacy Coordinating Committee. Reducing nontraumatic lower-extremity amputations by 20% by 2030: time to get to our feet: a policy statement from the American Heart Association. Circulation. 2021;143:e875–e891. doi: 10.1161/CIR.0000000000000967
2.Gornik HL, Aronow HD, Goodney PP, Arya S, Brewster LP, Byrd L, Chandra V, Drachman DE, Eaves JM, Ehrman JK, Evans JN, Getchius TSD, Gutiérrez JA, Hawkins BM, Hess CN, HoKJ, Jones WS, Kim ESH, Kinlay S, Kirksey L, Kohlman-Trigoboff D, Long CA, Pollak AW, Sabri SS, Sadwin LB, Secemsky EA, Serhal M, Shishehbor MH, Treat-Jacobson D, Wilkins LR.2024 ACC/AHA/AACVPR/APMA/ABC/SCAI/SVM/SVN/SVS/SIR/VESS guideline for the management of lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2024:1493.Diabetes Care 2024;47(Supplement_1):S231–S243
4.Thorud, Jakob, Mortality and Lower Extremity Amputation: What We Know Now, Podiatry today, April 2024
5.AbuRahma, Ali F, Clinical analysis and limitations of resting ankle-brachial index in the diagnosis of symptomatic peripheral arterial disease patients and the role of diabetes mellitus and chronic kidney disease, Journal of Vascular Surgery, Vol 71, No 3, March 2020
6.Raines, Jeffrey K., the Pulse Volume Recorder in the Diagnosis of Peripheral Arterial Disease, in Current Noninvasive Vascular Diagnosis, Aburama, Ali, PSG Publishing Company 1988
7.Lewis, J. Automated ankle brachial index measurement and pulse volume analysis compared to duplex scan, SAGE Open Medicine, 2016; Vol.4,1- v 71, No 9